- April 24, 2024
-
-
Loading

Loading
As the deadly hepatitis A virus continues to spread through the state, the Florida Department of Health has declared a state of emergency and has directed the departments of health in all 67 counties to vaccinate three populations who are at highest risk of contracting and spreading hepatitis A: homeless people, jail inmates, and anyone in drug rehab facilities. Volusia County's Department of Health has been busy.
"Our outreach teams are in the field visiting feeding sites and food pantries at churches and other social agencies, attending events that serve the at-risk groups, offering vaccinations at substance-abuse treatment facilities, sober houses, resource centers, etc.," Holly Smith, the health department's communications manager, wrote in an email. "They also have been on the street in areas frequented by the at risk populations, including parks and lodging sites suggested by law-enforcement and again offered vaccines on site to those interested."
Volusia is to be closely watched: It has the fourth highest rate of hepatitis A among Florida's 67 counties, with about 50 cases per 100,000 people.
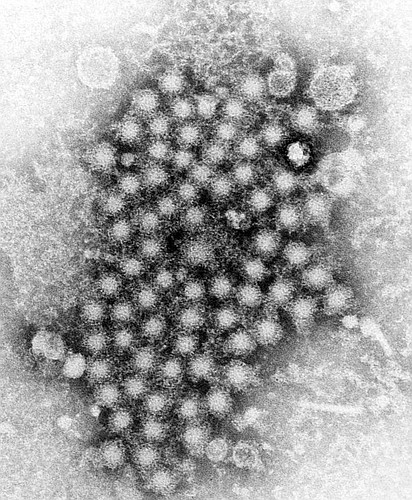
Hepatitis is an inflammation of the liver. Although the disease was discovered centuries ago, it was only in the past several decades that the five distinct strains — A, B, C, D and E — were been identified. Hepatitis A was first isolated in 1979, and vaccines were licensed in the mid-1990s, according to the Centers for Disease Control.
The hepatitis A virus has just one natural host: humans. It’s classified as an oral-fecal disease, meaning it’s acquired by mouth and spread through feces. Therefore, a common way for the disease to spread is for someone to neglect to wash his hands after using the restroom. He then could have the virus on his hand, and if he shares a cigarette, the virus could enter another person’s mouth.
After the virus incubates for five to 10 days, the infected person could have flu-like symptoms, have tea-colored urine or gray stools. Jaundice follows within days (the person’s eyes or face could have a yellow hue).
About three of every four people who get these symptoms require hospitalization, with a fatality rate of about 1.8% for patients who are older than 50.
In parts of the world with poor sanitation, about 90% have contracted the disease at some time in their lives; in industrialized countries, the rate is 33%, according to the “Control of Communicable Diseases Manual.”
There is no cure for hepatitis A. But vaccines and hand washing prevent it.
The Florida Department of Health declared a public health emergency on Aug. 1, 2019, because of an outbreak of hepatitis A statewide. There were almost 3,000 cases reported from Jan. 1 to Oct. 31, 2019, already about six times the total in all of 2018.
In response, the state created an incident command structure, providing additional resources and requiring each county to set goals and report on progress for administering vaccinations.
“It’s an all-hands-on-deck approach,” said Bob Snyder, director of the DOH in Flagler County.
Volusia has some help now with its efforts, with the jails now providing vaccinations to inmates. Also, hospitals offer the vaccinations to people who are over 65 with chronic health conditions. Volusia County government is working with municipalities "to discuss disinfection of public restrooms and shower facilities," Smith wrote in an email.
As of Nov. 1, 39% of the at-risk population had been vaccinated in Volusia County, which is better than the state average of 36%.
But, with the goal of vaccinating 80% of the at-risk population, there is much left to do.